Der Kardiovaskuläre Zwilling
Die Disruption der Gefäßdiagnostik
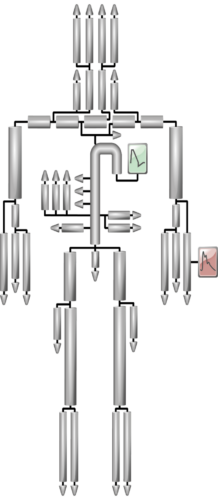
Im Nebel stochern war gestern! Zeitgemäße Diagnostik von Herz und Gefäßen verlässt sich nicht mehr auf althergebrachte und konventionelle Surrogatparameter wie z.B. die Pulswellengeschwindigkeit oder den Augmentationsindex. Wir messen die Gefäßsteifigkeit und den Gefäßwiderstand direkt in einem vom Individuum abgeleiteten, live simulierten Modell des menschlichen Arterienbaums.
Nicht-invasiv, KI-gestützt, jederzeit verlässlich reproduzierbar. Und vor allem:
In spektakulärer Präzision.






Pulssignaldiagnostik für Dummies
Was sind Pulswellen?
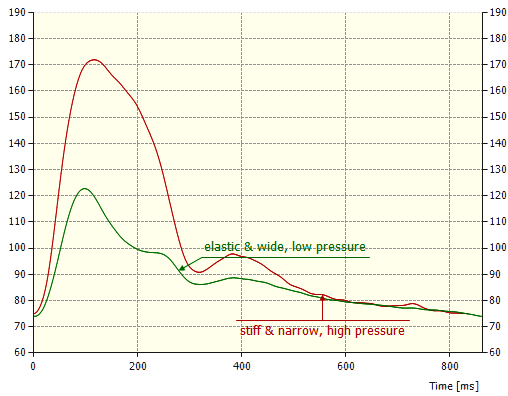
Pulswellen kommen dadurch zustande, dass das Herz als antreibender Motor das Blut stoßweise in den Arterienbaum befördert. Je nach Zustand des Herzens, und je nachdem, wie elastisch oder steif die Arterien sind, bilden sich unterschiedliche Druckverläufe in den jeweiligen Arterienabschnitten aus. Diese Puls-Druckverläufe nennt man kurz Pulswellen. Man kann sie fühlen, wenn man den Puls (zum Beispiel am Handgelenk) mit den Fingern ertastet.
Wozu Pulssignaldiagnostik?
Wenn das Herz krank ist oder aufgrund von Schwäche nur eingeschränkt arbeitet, und ebenso, wenn die Arterien mit der Zeit schlechter werden, hat dies einen drastischen Einfluss auf die Pulskurvenform. Wer die Pulssignale untersucht und ihre Form analysiert, weiß damit auch, wie es Herz und Arterien geht. Diese Kenntnis ist die wichtigste Basis für jegliche kardiovaskuläre Diagnostik und damit der bestimmende Faktor für die Erfolgsaussichten therapeutischer Interventionen. Im Gegensatz zu bildgebenden Verfahren wie Röntgen oder Magnetresonanz offenbaren Pulswellen die Funktionsfähigkeit von Herz und Arterien.
Die Überlegenheit des Kardiovaskulären Zwillings
Unsere Vision
Die auf künstlicher Intelligenz basierende, zum Patent angemeldete Methode der Herzkreislaufdiagnostik mittels Digital-Twin-Technologie ist in ihrer Form einzigartig. Sie hat enormes Potential, die kardiovaskuläre Diagnostik zu revolutionieren. Mit ihrer Vielfalt an mitgelieferten, klinisch relevanten Informationen stellt sie ein wichtiges Werkzeug für die Prävention, Akutdiagnostik, Therapie und Verlaufskontrolle von kardiovaskulären Fehlentwicklungen und Erkrankungen dar. Nach wie vor sterben weltweit Millionen Menschen an unentdeckten oder zu spät entdeckten kardiovaskulären Erkrankungen. Unser Ziel: Wir möchten unseren Teil dazu beitragen, dass sich das ändert. Deshalb muss der KI-basierte Herz- und Arteriencheck mit dem Kardiovaskulären Zwilling zur Standarddiagnostik der kardiovaskulären Prävention werden.
Pulswelle und biologisches Alter
Auch Arterien haben ein Verfallsdatum
Elastische Arterien mit ungehindertem Blutdurchfluss sind ebenso aus der Pulswelle ablesbar wie steife und verengte Gefäße, gegen deren zunehmenden Widerstand das Herz mit erhöhtem Druck anpumpen muss: Atherosklerose beginnt früher, als viele denken.